 Image from https://psychscenehub.com/
Image from https://psychscenehub.com/Trauma is a complex experience that can have long-lasting effects on the brain and body. When we experience a traumatic event, our brain and body undergo significant changes in response to the threat, which can lead to lasting physical and mental health consequences.
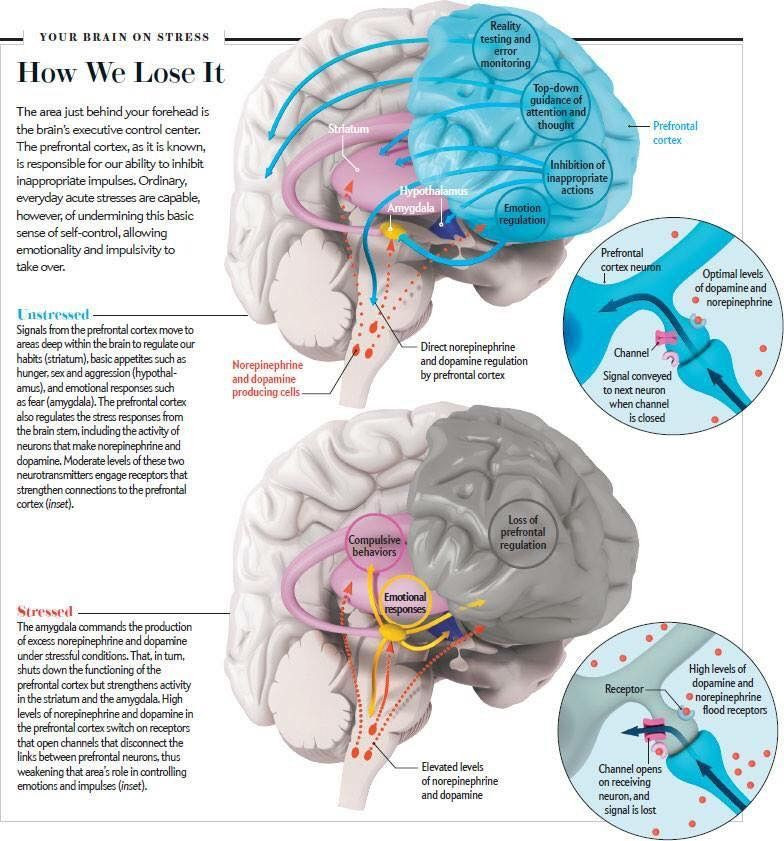
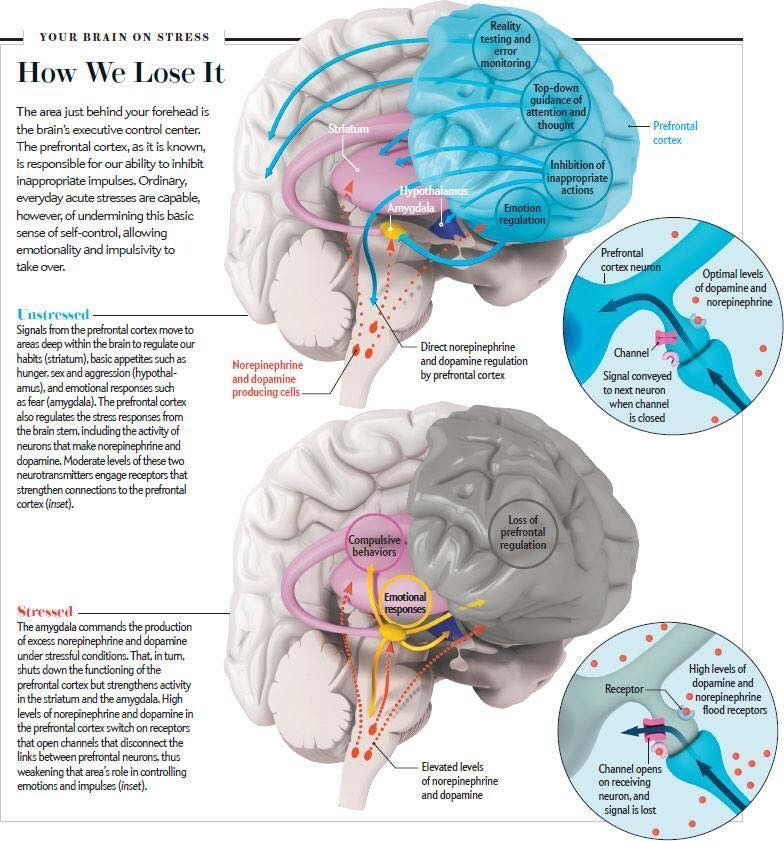
Recent research has shed light on the neurobiology of trauma, providing insight into how trauma affects the brain and body (Van der Kolk, 2015). Trauma can alter the structure and function of key brain regions, including the hippocampus, amygdala, and prefrontal cortex (Shin & Liberzon, 2010).
The hippocampus is responsible for forming and retrieving memories. Research has shown that trauma can lead to a decrease in the volume of the hippocampus, which can impact our ability to form and retrieve memories. This can lead to difficulties in recalling specific details of the traumatic event and can contribute to the development of post-traumatic stress disorder (PTSD) (Yehuda et al., 2006).
The amygdala is responsible for processing and responding to emotional stimuli. Research has shown that trauma can lead to an increase in the activity of the amygdala, which can lead to an exaggerated fear response. This can contribute to the development of anxiety disorders and can make it challenging to manage emotions related to the traumatic event (Shin & Liberzon, 2010).
The prefrontal cortex is responsible for executive functioning, including planning, decision-making, and impulse control. Research has shown that trauma can lead to a decrease in the volume of the prefrontal cortex, which can impact our ability to regulate our emotions and make sound decisions. This can contribute to the development of impulsive behaviors and difficulty managing emotions related to the traumatic event (Shin & Liberzon, 2010).
The Impact of Trauma on the Brain
One of the most significant ways that trauma impacts the brain is by altering the structure and function of key brain regions. Research has shown that trauma can lead to changes in the hippocampus, amygdala, and prefrontal cortex, all of which play critical roles in our ability to process and respond to information (Shin & Liberzon, 2010).
The hippocampus is responsible for forming and retrieving memories. Research has shown that trauma can lead to a decrease in the volume of the hippocampus, which can impact our ability to form and retrieve memories. This can lead to difficulties in recalling specific details of the traumatic event and can contribute to the development of post-traumatic stress disorder (PTSD) (Yehuda et al., 2006).
The amygdala is responsible for processing and responding to emotional stimuli. Research has shown that trauma can lead to an increase in the activity of the amygdala, which can lead to an exaggerated fear response. This can contribute to the development of anxiety disorders and can make it challenging to manage emotions related to the traumatic event (Shin & Liberzon, 2010).
The prefrontal cortex is responsible for executive functioning, including planning, decision-making, and impulse control. Research has shown that trauma can lead to a decrease in the volume of the prefrontal cortex, which can impact our ability to regulate our emotions and make sound decisions. This can contribute to the development of impulsive behaviors and difficulty managing emotions related to the traumatic event (Shin & Liberzon, 2010).
The Impact of Trauma on the Stress Response System
Trauma can also impact the stress response system, which is responsible for helping us respond to and cope with stressful situations. When we experience a traumatic event, our stress response system is activated, leading to the release of stress hormones such as cortisol and adrenaline (McEwen, 1998).
In individuals who have experienced trauma, the stress response system can become dysregulated, leading to a heightened state of arousal and increased sensitivity to stress (McEwen & Gianaros, 2010). This can contribute to the development of anxiety and other stress-related disorders and can make it challenging to manage daily stressors.
Additionally, research has shown that trauma can lead to alterations in the immune system, which can impact our physical health. Individuals who have experienced trauma may be more susceptible to developing chronic health conditions such as autoimmune disorders and cardiovascular disease (McEwen, 2012).
Yoga and mindfulness techniques can help you learn to regulate your nervous system and reduce stress (Khalsa & Cope, 2006). Meditation and breathwork exercises can also help you manage stress and improve emotional regulation (Ramesh, Marimuthu, & Krishnamurthy, 2018). In addition, proper nutrition and regular exercise can improve your overall health and help you manage the physical and mental health consequences of trauma (Gómez-Pinilla, 2008; Miller & Raison, 2016; Stubbs et al., 2017).
If you're interested in learning more about how holistic health coaching can help you live with the effects of trauma, contact me for a free consultation. Together, we can work towards achieving your health and wellness goals.
Be sure to Subscribe to learn more about how trauma can impact your brain and body and self-care activities to improve your resilience.
References:
J. D., Yehuda, R., Grossman, R., New, A. S., Mitropoulou, V., & Siever, L. J. (2005). Childhood trauma and basal cortisol in people with personality disorders. Comprehensive Psychiatry, 46(2), 103-107. doi: 10.1016/j.comppsych.2004.06.008
McEwen, B. S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338(3), 171-179. doi: 10.1056/NEJM199801153380307
McEwen, B. S. (2012). Brain on stress: How the social environment gets under the skin. Proceedings of the National Academy of Sciences, 109(Supplement 2), 17180-17185. doi: 10.1073/pnas.1121254109
McEwen, B. S., & Gianaros, P. J. (2010). Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Annals of the New York Academy of Sciences, 1186(1), 190-222. doi: 10.1111/j.1749-6632.2009.05331.x
Shin, L. M., & Liberzon, I. (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology, 35(1), 169-191. doi: 10.1038/npp.2009.83
Taylor, S. E., Way, B. M., Welch, W. T., Hilmert, C. J., Lehman, B. J., & Eisenberger, N. I. (2006). Early family environment, current adversity, the serotonin transporter promoter polymorphism, and depressive symptomatology. Biological Psychiatry, 60(7), 671-676. doi: 10.1016/j.biopsych.2006.03.070
Van der Kolk, B. A. (2015). The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin.
Yehuda, R., Flory, J. D., Southwick, S., & Charney, D. S. (2006). Developing an agenda for translational studies of resilience and vulnerability following trauma exposure. Annals of the New York Academy of Sciences, 1071(1), 379-396. doi: 10.1196/annals.1364.029


0 Comments